Trauma & PTSD
What does exploring trauma look like in therapy? Many therapists have different thoughts and approaches when working with trauma. I have had many clients initiate trauma focused therapy with me because of frustration that they felt no substantiative relief from past talk therapies. I has extensive training in trauma and trauma-informed approaches. I know, as Dr Peter Levine states, “Trauma is in the nervous system, not in the event.” I trained in many techniques and therapies that can hone in on beneficial starting points for trauma treatment, work to activate the body to move toward adopting new ways of feeling, thinking, and sensing of past triggering events.
There are different types of trauma including singe incident, complex, and developmental trauma. Single incident trauma are such events as accidents, natural disasters, single abuse/assault incidents, sudden loss, witnessing violence, or illness or medical issue. Complex trauma includes histories with on-going abuse(s) or neglect, domestic or community violence, bullying, war, betrayal, or abandonment. Developmental trauma is always complex trauma. Developmental trauma is especially focused on the 0-5 years old range with hurts or omissions from caregiving sources. Many times, this trauma is not exactly what happened but what was missing in childhood such as, not have feelings or situations validated as traumatic, not having a sense of connection, love, or protection.
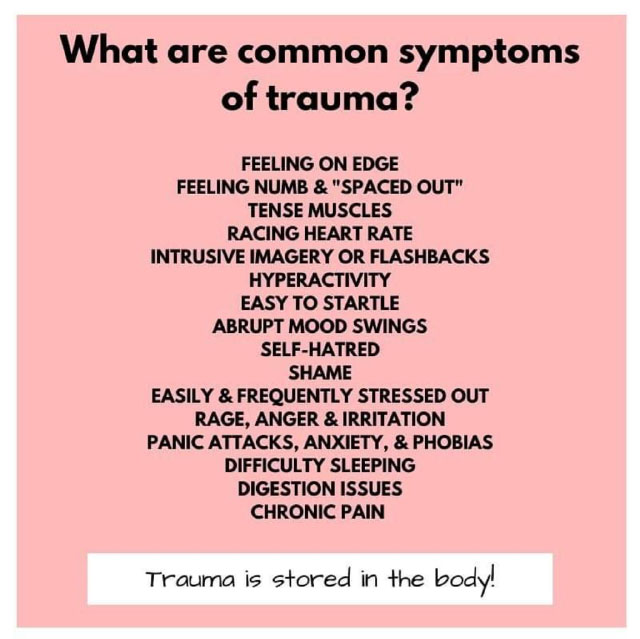
All traumas can lead to poor self-identity and shame. Understanding the underlying core beliefs (negative self-talk) is an important piece of working through trauma.
How long trauma therapy can take depends on a lot of factors and cannot be predicted. A past client post 9/11/2001 asked, “How come some of my colleagues are going back to work and I can’t leave my closet?” My reply was to not compare apples to oranges. Different people’s life experiences (past traumas), brain make-up or chemistry, support system, etc. can play into some of the factors that determine length and complexity of treatment.
Some single incident traumas can be resolved or neutralized in trauma focused therapy in 3-10 sessions. The more chronic the trauma was experienced the longer trauma treatment can take. But in the long run, making the investment in trauma treatment can help you be able to feel physical and emotional relief, be less triggered in present day situations that may have some of the same themes/nuances, and learn to be kinder to yourself.